Omega-3 fatty acids, commonly found in fish oil, have long been promoted as a cornerstone of heart health.
The promise of preventing heart disease and reducing inflammation led many, myself included, to add omega-3 supplements to our daily routines.
But after digging deeper into the research and seeing both the benefits and risks, I’ve made a personal choice to stop taking them. Here’s why I’ve made this decision, and why you might want to rethink your omega-3 supplement use too.
What Are Omega-3 Fatty Acids?
Omega-3 fatty acids are a type of polyunsaturated fat that are essential for many body functions, particularly the heart.
The most important types of omega-3s are:
- Eicosapentaenoic acid (EPA): Typically found in fish, EPA is believed to have anti-inflammatory properties and may help reduce cardiovascular risk.
- Docosahexaenoic acid (DHA): Also found in fish, DHA plays a critical role in brain function and vision, but it’s also thought to benefit the heart.
- Alpha-linolenic acid (ALA): Found in plant sources like flaxseeds, flaxseed oil, and walnuts, ALA can be converted to EPA and DHA, but the conversion process is not very efficient.
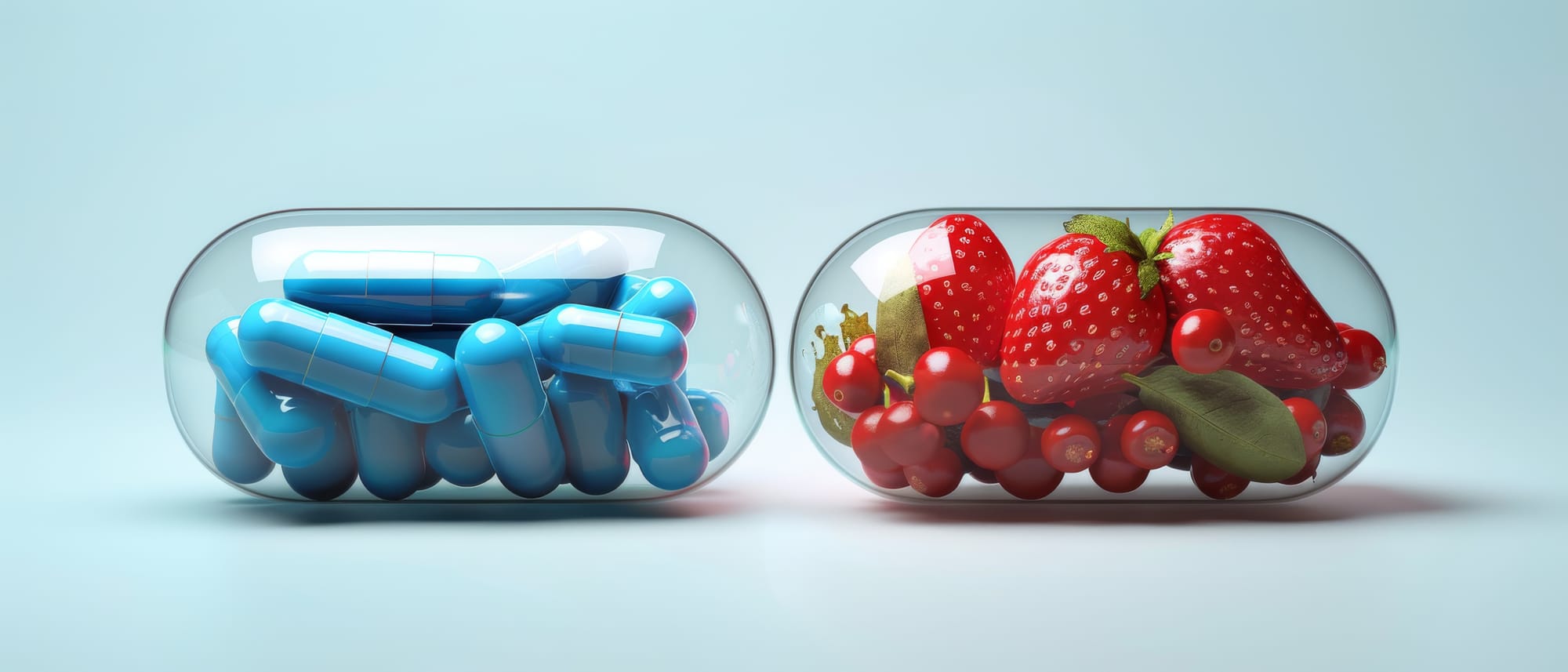
For years, omega-3 supplements, especially those containing EPA and DHA, have been marketed as a one-stop solution for improving heart health and preventing cardiovascular events like heart attacks and strokes. But the more I looked into it, the more I realized that these supplements might not be the magic pill they’ve been made out to be.

The Early Promise of Omega-3 Fish Oil: What Got Us Hooked
Back in the 1990s, early research suggested that people who ate a lot of seafood had lower rates of heart disease, particularly sudden cardiac arrest. This led scientists to believe that omega-3 fatty acids in fish might have protective effects on the heart. From there, omega-3 supplements took off, and for good reason: why not take an easy pill that promises the same benefits as eating fish?

However, most of these studies focused on people who consumed omega-3s through their diet—primarily fish. It is important to eat fish as a primary source of omega-3 fatty acids because whole foods provide a broader range of nutrients that supplements alone cannot match.
While that might make you think that popping fish oil capsules would have the same effect, it turns out the science doesn’t back that up.
What Recent Studies Have to Say: A Mixed Bag
Although some early studies hinted that omega-3s might lower the risk of heart disease, recent studies have painted a more complicated picture.

- The VITAL Study: One of the largest and most important studies on omega-3s, this trial looked at over 25,000 people and found no significant reduction in major cardiovascular events—like heart attacks or strokes—among those taking omega-3 supplements compared to a placebo.
- High-Dose EPA Study: In contrast, another study found that a high dose of EPA (2000mg twice a day) did reduce the risk of heart events, but this was in a very specific group of people—those with high triglycerides and already taking statins for heart disease. However, this benefit wasn’t seen when EPA was combined with DHA, the typical formula found in over-the-counter fish oil supplements.
The Atrial Fibrillation Link: A Risk You Can’t Ignore
One of the most concerning findings that tipped the scales for me was the link between omega-3 supplements and atrial fibrillation (AFib)—a type of irregular heartbeat. AFib isn’t just a mild inconvenience; it increases your risk of stroke and other serious heart issues.

A recent analysis that looked at five major studies found that people taking omega-3 supplements had a 37% higher risk of developing AFib compared to those taking a placebo. While the absolute increase in risk was small (from about 1.94% to 2.65%), it was enough to make me reconsider whether the potential benefits outweighed this newly discovered risk.
Interestingly, this increased risk of AFib was seen mostly in people who were already at high risk for heart disease. If omega-3 supplements can trigger an irregular heartbeat in people who are already vulnerable, that raises important questions about whether they’re safe for everyone.
Why Whole Foods Trump Supplements
One thing that stood out to me in my research was that getting omega-3s from food seems to offer better and more consistent benefits than taking supplements.
For example, eating fatty fish like salmon, mackerel, and sardines has been shown to improve heart health without the risks associated with high doses of omega-3 in fish oil pills.

When we eat whole foods, we’re not just getting omega-3s. We’re also consuming a wide range of other nutrients and antioxidants that work together to support our body. This balance is often lost when you isolate a nutrient, package it into a pill, and take it in large doses. Plus, food sources of omega-3s come with other important nutrients, like vitamin D and high-quality protein, that support overall health.
Do Omega-3 Supplements Still Have a Place?
I’m not saying omega-3 supplements are useless. For certain groups—such as people with very high triglycerides or those who can’t consume fish—there may still be a role for omega-3 supplements. But for the average person looking to protect their heart, the evidence just doesn’t support popping a pill as a cure-all.
Moreover, because the data on omega-3 supplements is so mixed, individualized healthcare is crucial. If you’re considering or already taking fish oil supplements, talk to your doctor about your personal heart health and any risks you might face, including AFib.
My Takeaway: Food First, Supplements Second
After considering the research, I’ve decided to take a food-first approach to getting omega-3s. Instead of relying on supplements, I make sure to eat fatty fish a couple of times a week, and I also incorporate plant-based omega-3s like flaxseeds, chia seeds, and walnuts into my diet.
This approach feels more balanced and less risky, and it aligns with the recommendation from many health organizations to prioritize whole foods over supplements. After all, nature provides us with everything we need if we make thoughtful choices about what we eat.

Make an Informed Choice
At the end of the day, whether or not to take omega-3 supplements is a personal decision. For me, the risk of AFib combined with the mixed research on heart benefits led me to stop. But that doesn’t mean omega-3 supplements aren’t right for everyone. It’s important to weigh the risks and benefits based on your own health needs.
If you’re unsure, talk to your healthcare provider about what’s best for you. And remember, while supplements can be helpful in some cases, they’re no substitute for a well-rounded diet rich in whole, nutritious foods.
Disclaimer: This post is for informational purposes only and does not constitute medical advice. Always consult with your healthcare provider before making any changes to your health routine.



